Living 3D skin models for the study of skin diseases

The new 3D skin model will allow scientists to simulate skin diseases and thus better understand them.
Swiss researchers are developing a new material that enables the production of living 3D models of human skin.
The cultivation of cells in a laboratory setting is a well-established practice. However, the reconstruction of entire tissues poses a greater challenge. This would be of significant benefit to the over 1,500 known skin diseases, enabling more effective understanding and exploration of new therapeutic approaches. Researchers at the Swiss Federal Laboratories for Materials Science and Technology (Empa) are therefore developing a new material based on hydrogel that allows the creation of living three-dimensional models of human skin.
The project is part of the Swiss research initiative SKINTEGRITY.ch, the aim of which is to better understand what happens in the skin at a molecular level during injury, healing or disease. The skin is the largest organ of the human body, accounting for around 15% of total body weight. Although conditions such as skin cancer, chronic wounds and autoimmune skin diseases are widespread, there is still limited knowledge about why they arise.
A step closer to artificial human skin
To find answers, Empa researchers are working together with doctors on a model of human skin that can be used to simulate skin diseases for better understanding. According to the press release, the objective of the researchers is to produce a living ‘artificial skin’ that contains skin cells and emulates the layered, wrinkled structure of human skin.
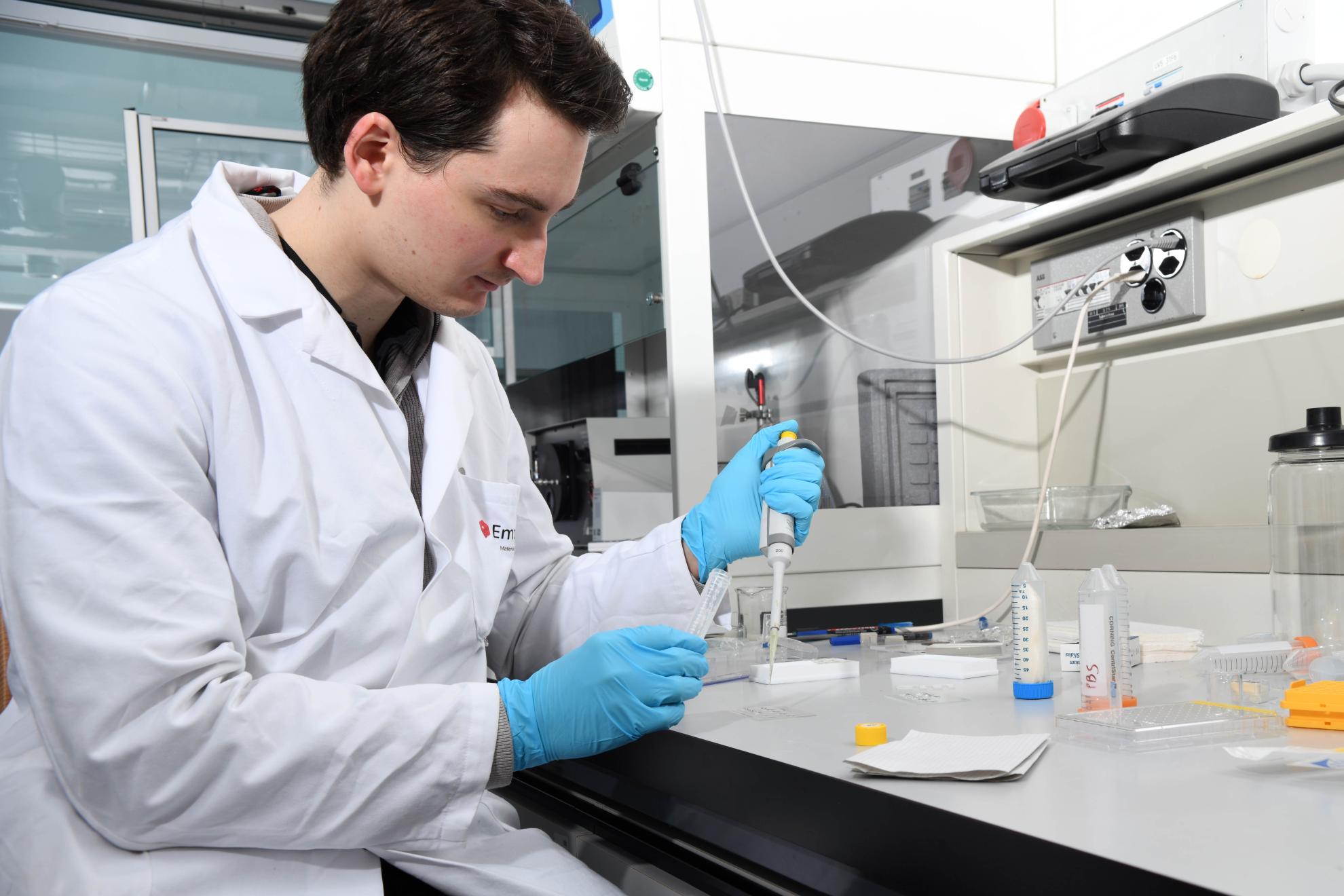
Empa researchers are working together with clinical partners on a model of human skin.
Gelatine derived from cold-water fish
In order to successfully reconstruct human skin, researchers must first identify suitable building materials. The Empa team has recently made significant progress in this area, developing a hydrogel that meets the complex requirements and is also easy to produce. The base material is gelatine derived from the skin of cold-water fish. Gelatine from cold-water fish, such as cod, pollock and haddock, can be cross-linked with ease to form a non-swelling hydrogel that can be printed together with skin cells.
Fish skin is currently being researched as a promising tool for wound healing.
The future of wound dressings
As fish are evolutionarily more distant from humans, fish gelatine causes fewer immune reactions and carries a lower risk of disease transmission compared to similar materials based on mammalian gelatine, according to the researchers. The resulting material is also biologically compatible with human skin cells, which opens the door to future use as wound dressing material. The successful patent application marks the initial step in this direction.




