Healing from within: scientists discover gut bacteria that regenerates the colon
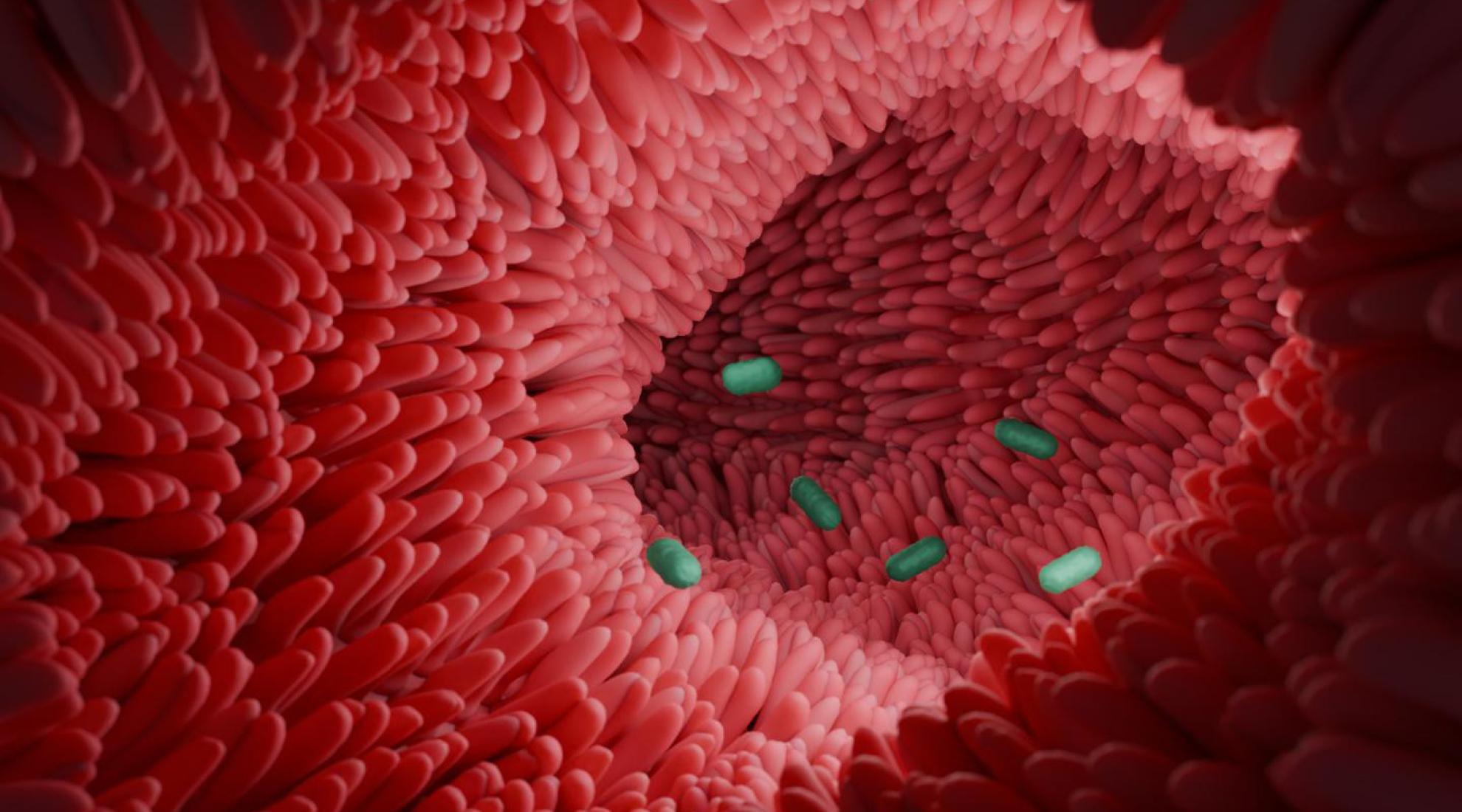
An illustration of the Clostridium scindens bacterium in the intestine.
EPFL scientists have discovered that a special gut bacterium helps regenerate the colon by balancing bile acids – offering hope for treating diseases like ulcerative colitis.
A team of researchers led by EPFL has made a significant breakthrough in gut health. Their discovery centres around Clostridium scindens, a gut-dwelling bacterium capable of regenerating the colon's inner lining. This research has the potential to revolutionise the treatment of diseases such as ulcerative colitis (UC) – a chronic condition estimated to affect 5 million people worldwide.
Rather than attacking inflammation directly, C. scindens appears to support the body’s natural ability to repair damaged intestinal tissue. It does so by transforming primary bile acids, which are typically associated with fat digestion, into a specific form that triggers regenerative responses in the colon.
From digestion to regeneration
The key to this process lies in the transformation of bile acids. The liver produces primary bile acids to help digest fats. However, when C. scindens is present in the gut, it converts these primary acids into what are known as 7α-dehydroxylated bile acids.
These converted bile acids activate the TGR5 receptor, a protein found in various tissues throughout the body, including the gastrointestinal tract, liver, and brain. Once stimulated, the TGR5 receptor begins promoting the regeneration of damaged tissue in the colon. The researchers tested their hypothesis in mice with colitis, a disease model similar to UC. The results show that the presence of C. scindens significantly accelerated healing and reduced inflammation.
Our findings highlight the potential of microbiome-targeted strategies to modulate bile acid metabolism and promote gut healing.
A new era in gut disease therapy
Current treatments for UC often rely on suppressing inflammation with the help of immunosuppressants or biologic medicines, which aim to reduce the activity of the immune system or the proteins responsible for stimulating inflammation, respectively. It goes without saying that weakening the immune system can automatically lead to more serious side effects.
EPFL’s discovery opens the door to an entirely different kind of treatment – one that works in harmony with the body's own biology and addresses the root cause of the condition. With the help of the bacterium C. scindens in the gut and its subsequent lower levels of certain bile acids, it may be possible to support natural healing without the need for harsh pharmaceutical interventions. Researchers are optimistic that this could lead to new probiotic-based therapies that are a more sustainable option for patients.
What comes next?
While these findings are promising, the journey from lab bench to bedside is still ongoing. Further studies are needed to explore its clinical applications, and how its effects might differ across individual patients. If successful, it could mean a better quality of life for patients suffering from chronic intestinal diseases.




